Background: Avascular necrosis (AVN) afflicts up to 10% of patients with sickle cell disease (SCD), and results in significant impairment in mobility and quality of life. The femoral head is the most common site for involvement of AVN in SCD patients. Total hip arthroplasty has a higher rate of perioperative complications in SCD patients, when compared to the general population. In this study, we aimed to evaluate the rates of readmissions in SCD patients undergoing hip arthroplasty as well as examine the causes behind these readmissions.
Methods: The Nationwide Readmissions Database (NRD) was queried to include all adults who underwent hip arthroplasty in the years 2016 and 2017. SCD patients with AVN of the hip were compared to those undergoing hip arthroplasty for other reasons. T-test was used to compare means of continuous variables and Chi-square test to compare proportions of categorical variables. Multivariable logistic regression was used to evaluate risk factors for inpatient mortality, increased length of hospital stays, and hospitalization charges. We also examined risk factors for readmissions and the most common causes of readmissions in both sickle cell and non-sickle cell cohorts.
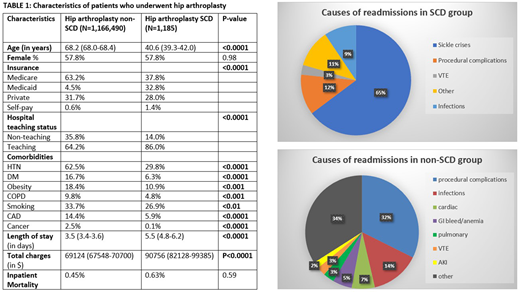
Results: A total of 1,167,675 hip arthroplasties were performed in 2016 and 2017, of which 0.1% were for SCD patients with AVN. As expected, those with SCD were younger (mean age 40.6 vs 68.2 years, p<0.0001), with an equal gender distribution (57.8% female) in the two groups. Sickle cell patients were more likely to be from lower income neighborhoods and were also more likely to be treated at teaching hospitals. After adjusting for demographic variables and comorbidity burden, sickle cell disease was associated with higher risk of inpatient mortality (aOR 9.50, 95% CI 2.39-37.77, p<0.01), longer length of hospital stay by 3.2 days (95% CI 2.5-3.9 days, p<0.001), and higher hospitalization costs by roughly 20,000 USD per admission (95% CI 12,000-29,000 USD, p<0.001).
On multivariate analysis, sickle cell patients were more likely to be readmitted within 60 days (aOR 5.25, 95% CI 4.01-6.87, p<0.001). 65% of these readmissions were due to SCD itself. Procedural complications resulted in a 60-day readmission rate of 3% in both the SCD and non-SCD groups, whereas, infectious complications accounted for a higher rate of readmission in those with SCD (2.4% vs 1.3%).
Conclusions: Hip arthroplasty is associated with inferior inpatient outcomes and higher resource utilization in those with sickle cell disease. This can be attributed to high incidence of sickle cell crises post-procedure, as well as, intraoperative surgical complications (femoral fractures and perforations) and high rates of postoperative infections in the functionally asplenic sickle cell disease population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal